Encephalitis
What is Encephalitis?
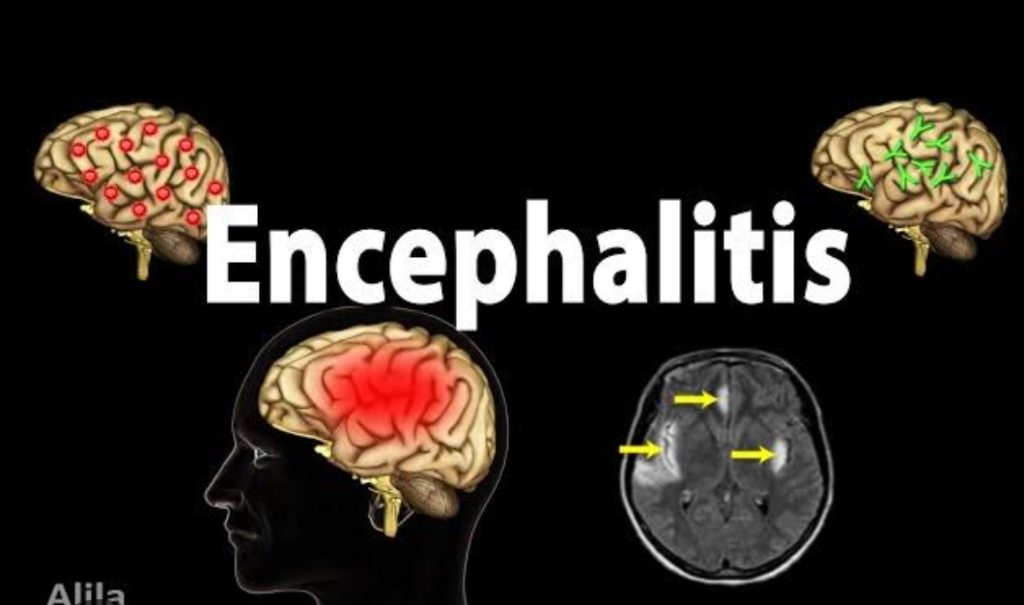
Encephalitis is a condition where the brain develops an inflammation around it. There are many possible causes, but the most common cause is a viral infection.
Due to the inflammation in the brain, it exerts pressure to the skull and the contents inside and may cause moderate symptoms – like headache or fever or may display no symptoms in any way. Sometimes, the symptoms may be acute and encephalitis may bring about problems with motion or sensations, seizures, or even thinking.
Encephalitis could be life-threatening and timely treatment and identification are important as it is hard to forecast how each person will be affected by encephalitis.
Assessment
Headache
Fever
Aches in joints or joints
Fatigue or weakness
Confusion, agitation or Illness
Seizures
Reduction of sensation or paralysis in certain Regions of the body or face
Muscle fatigue
Issues with hearing or speech
Reduction of awareness
In young babies and smaller children, the signs and symptoms may include:
Bulging, visible at the soft spots or fontanels of a baby’s skull
Nausea and vomiting & Irritability
Poor feeding or never awakening to get a feeding
Body stiffness
Causes of Encephalitis
The cause of encephalitis is still not very clearly established. However, amongst the commonest understood causes, the most frequent is a viral disease. Infections and illnesses that are non-infectious may also lead to encephalitis.
There are two types of encephalitis:
Main encephalitis – This condition happens when a virus or other representative directly infects the brain. The disease might be concentrated in 1 place or may be widespread. A key infection might lead to the reactivation of a virus that was earlier dormant.
Secondary encephalitis – This illness results in a faulty immune system response to an infection elsewhere in the body. Rather than attacking the cells of the immune system, the illness also attacks healthy tissues from the brain. Secondary encephalitis usually happens after the disease.
Frequent viral triggers Include:
Herpes simplex virus (HSV). The two HSV type
Type 1 – Related to cold sores and fever and blisters around the mouth
Type 2 – Related to genital herpes – may lead to encephalitis.
Encephalitis is rare but can lead to death or brain damage.
Other herpes viruses – These include the Epstein-Barr virus, which causes infectious mononucleosis, and the varicella-zoster virus, which causes chickenpox and shingles.
Enteroviruses – These viruses comprise the poliovirus and coxsackievirus, which results in illness with flu-like symptoms, eye discomfort, and stomach pain.
Mosquito-borne viruses – These germs may cause infections like West Nile, La Crosse, St. Louis, western equine and eastern equine encephalitis. Signs of a disease might appear following exposure to some viruses within a few weeks.
Tick-borne viruses – The Powassan virus is carried by ticks and causes encephalitis. Symptoms typically appear about a week following a bite from an infected tick.
Rabies virus – Infection with the rabies virus, which is typically transmitted by a bite from an infected animal, triggers a rapid progression to encephalitis when symptoms start. Rabies is an uncommon cause of encephalitis in some places.
Childhood infections – Common childhood illnesses – like measles rubeola, mumps, and German measles or rubella – used to be quite common causes of secondary encephalitis.
Diagnostic test for Encephalitis
Body fluid tests – This test might include a fluid sample from the throat, nose, blood or even bowel movement. The test results might indicate which particular germ is triggering the illness.
Neurologic exam – A neurologic exam can show how well the brain functions after an illness or injury. The medical examiner will check how the patient’s pupils respond to light. He/she might check their memory and how effortlessly the person is able to wake up. The balance and hand grasp might be tested as well.
Nursing responsibility
Assess conscious level of the patient.
Evaluate the neurology status every 1-2 hours and when required until the individual reaches a steady condition.
Evaluate the level of pain.
Monitor vital signs.
Elevate the bed head to 30 ° and help the head and throat to improve venous return.
Preserve a comfortable and quiet environment.
Check signs of septic shock (increased temperature, hypotension, increased RR, disorientation, confusion, peripheral vasoconstriction).
Administer prescribed medication

