Seizure Disorder
A seizure is the interruption of normal brain functioning by uncontrolled paroxysmal discharge of electrical stimuli from the neurons.
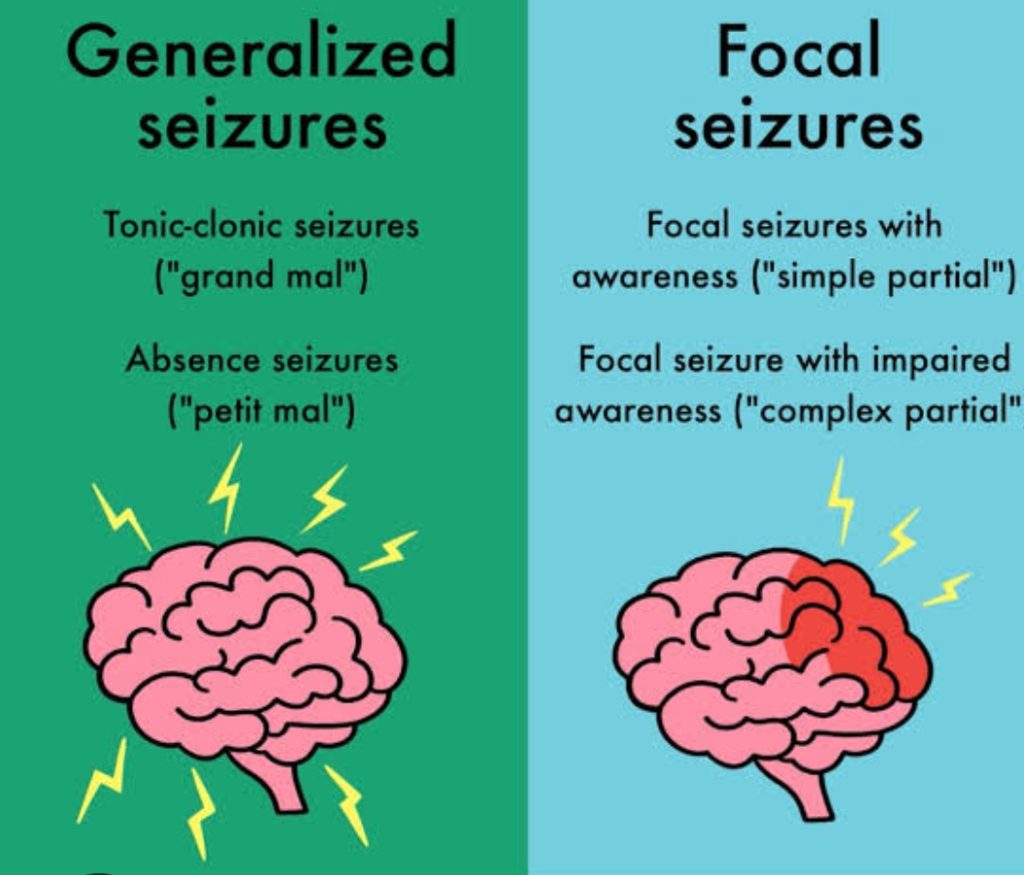
Seizures occur when abnormal electrical signals are being rapidly fired for neurons in the brain. This can happen throughout the brain affecting both sides (generalized seizure) and being located in a specific area of the brain (partial or focal seizure).
Seizures can occur in anyone (children and adults) due to a severe acute condition, such as a high fever, illness (especially central nervous system types like bacterial meningitis), hypoglycemia, acid-base imbalances like acidosis, alcohol withdraw, brain tumor etc. Once the condition is corrected the seizures tend to stop.
Simplified Pathophysiology of Seizures
In the brain, our neurons are tasked with handling and transmitting information. There are two types of neurons I want to discuss. These are excitatory and inhibitory neurons. Just like their name says, excitatory neurons produce “an action” or cause “excitement” by releasing a neurotransmitter called glutamate (this is an excitatory neurotransmitter).
Inhibitory neurons “stop an action” or cause inhibition by releasing an inhibitory neurotransmitter called GABA.
For seizure activity not to occur in a healthy brain, there needs to be a proper balance between these two types of neurons. If there is an imbalance of excitatory neurons vs. inhibitory neurons seizures will occur. For example, if there is not enough GABA (remember this is the inhibitory neurotransmitter) being released, too much excitation will occur leading to seizure activity.
Knowing the causes of seizure will help one understand how some of the anti-seizure drugs work to treat seizures. For instance, barbiturates stimulate GABA receptors which help control excitation and decrease seizure activity (more about medications below).
Types of Seizures
1. Generalized: seizure affects both parts of the brain Tonic-clonic (formerly called grand-mal): most common type of generalized seizure
May experience AURA (warning a seizure is about to happen)
Loses consciousness (at risk for injury)
Will experience a tonic phase: body stiffens (may bite inside of the cheek or tongue….may see blood leaving the mouth with foaming of saliva), breathing stops followed by cyanosis)
Then a clonic phase: recurrent jerking (spasm and relaxation back-to-back) of extremities (patient may have incontinence of stool or/and urine)
Usually lasts no more than 3 minutes…..at risk for status epilepticus with this type of seizure
NOTE:if greater than 5 minutes or having multiple seizures in a row, activate the emergency response team (will need immediate treatment to stop the seizure (more on this in the nursing interventions)
Post ictus (duration: hours to days): this is the recovery period: The patient will feel very tired, extremely sore from muscle stiffening and jerking, and can’t remember what happened.
Tonic seizure: (stiffening of the body at risk for falling) or Clonic seizure: (jerking can be symmetrical or asymmetrical)
Absence Seizure (formerly called petit-mal)
Most common in pediatric patients and Hallmark is a staring- like state
It will be like the child is just daydreaming but can’t be snapped out of it, can go unnoticed by others for a while because it is short and the child won’t remember it. The person will look confused and won’t be able to talk during the event. Last within seconds. Post Ictus: immediate…doesn’t remember staring off
Atonic seizure (drop attacks):
WITHOUT MUSCLE TONE
The patient goes limp and falls if standing or slumps over if sitting…at risk for head injury (may need a helmet) and is usually not aware during the event.
Post ictus: is immediate and regains consciousness
Clonic seizure
Hyperventilation, with rapid jerking movements. Tongue biting, incontinence, and heavy salivation may occur during this period
Myoclonic seizure:
Quick duration of jerking of the muscles
The patient is usually aware and conscious (this is what makes it different from a clonic seizure)
It lasts for a Very short (a few seconds).
Focal (also called partial): affects a specific part of the brain. Focal Onset AWARE (simple partial): symptoms vary depending on where the seizure is located. It tends to be a small area of a lobe, but the patient is AWARE…example: occipital region the person may have vision changes.
Also sometimes called an aura too because it can happen right before focal impaired awareness (complex partial)
Stages of Seizure
We can divide how a person experiences a seizure it can be divided into stages (it varies depending on the seizure type)
Prodromal: when symptoms start to appear prior to the big event (hence seizure), can start days before a seizure happens, mood changes (depression, anger, issues sleeping, anxiety, GI and urinary issues etc.)
Aura: This doesn’t happen with all types, happens at the very beginning of the seizure (what type: focal seizures OR in a tonic-clonic seizure), happens within seconds to minutes before a seizure many times it gives the patient time to prepare self for seizure. As the nurse (if you are present) help the patient lay down on their side with a pillow under the head.
Symptoms vary among patients but can include: a sudden weird smell or taste, déjà vu feeling, feeling anxious like something bad is about to happen, altered vision (lights or spots in vision) or hearing (hallucination type sounds or increased ability to hear sounds), dizzy (different for every person), inability to speak etc.
Ictus: (word means seizure) This is the actual seizure
Usually lasts anywhere from 1 to 3 minutes
Seizures greater than 5 minutes or if the patient starts having seizure back-to-back, the patient may be experiencing status epilepticus (will need medical care and medication to make the seizure stop…it will unlikely stop on its own)
Post Ictus: (after the seizure) brain is going to rest and recover from the seizure usually last hours to days (tonic clonic) for some patients it is immediate (absence seizure), may feel extremely tired, sleepy, confused, headache etc.
Nursing Interventions for Seizures
Assess risk factors for seizure. If risk factors present initiate seizure precautions:
Seizure precautions may include:
At bedside have suction and oxygen ready
IV access (to given anti-seizure medication, if needed)
Padded side rails
Pillow under head (to protect head)
Bed in the lowest position
If patient is able to report prodromal or aura, assist the patient prepare by getting the patient in a safe position by lying down on their side.
What to do when your patient has a seizure?
Protect patient if they are standing-up or sitting down by:
Gently lying the patient down and turning them onto their side. This helps to prevent the tongue from covering the airway and helps saliva and blood drain from the mouth.
DO NOT restrain patient or try to hold the patient down
Protect their head and extremities (pillow and bed pads will help with this)
DO NOT put anything in the patient’s mouth
Remove anything that can impede breathing or break (eye glasses, tight clothing etc.
Note the time it started and time it stopped (VERY IMPORTANT: if greater than 5 minutes or another seizure happen .THINK: status epilepticus and activate the emergency system response team.
You will notify the HCP of the seizure regardless because the seizure needs to be investigated.
When the seizure started what was the patient’s behavior right before and during it? (did they cry out, become confused, report an aura, become unconscious) and the characteristics of the body movements (if any) presented at the beginning and throughout the seizure, stiffening of the whole body or just the extremities and then jerking or just jerking, was it on just one side or both sides of the body, be sure to be as detailed as possible, this helps the healthcare team determine what type of seizure this was and what treatment may be needed
Did the patient become incontinent of urine or stool?
Oxygen status (cyanosis present)
Nurses role during the Post Ictus stage:
Note the time the seizure stopped and how the patient is behaving afterwards:
Are they tired (let them sleep and rest), confused, can’t think or talk, have a headache (ask where it is located and pain rating), has any injuries (some patients may bite their tongue or cheek)
Maintain airway (suction, administer oxygen)
If a tonic-clonic seizure, the patient will be very sleepy, and won’t remember what happened.
Assess vital signs and neurological status: pupils, reflexes, is patient confused or oriented
Clean patient if incontinence was experienced.
Document and report it to the HCP,is this your patient’s first seizure, are they on anything for seizures (is drug level not therapeutic….may need to draw a drug level if ordered by HCP)
Electro Encephalo Gram(EEG) may be ordered: to assess brain activity.
EEG investigation
It is a Painless procedure.
Hold seizure medications or medications that are stimulants or depressants before EEG (these medications can prevent the proper assessment of abnormal brain waves associated with a seizure)
No caffeine products (a stimulant) 8 hours before
Can eat before
Medications/Treatments
Medications is based on the type of seizure:
Barbiturates: Phenobarbital (used tonic-clonic or focal seizures & status epilepticus), stimulates GABA receptors & this helps inhibitory neurotransmission
Side effects: drowsiness, uncoordinated movements (ataxia) etc.
Watch for: respiratory depression and hypotension
Drug level 15 to 40 mcg/mL
Hydantoins: Phenytoin (used in tonic-clonic or focal seizures)
watch the gums: will enlarge and easily bleed (called gingival hyperplasia….teach about good mouth hygiene
phenytoin, may cause bone marrow suppression (watch platelets and WBCs)
inform patient to watch for rash or Steven-Johnson’s Syndrome and to REPORT it immediately
Don’t give with milk or antacids (interferes with absorption)
10 to 20 mcg/mL
Benzodiazepines: For absence seizures, tonic clonic, focal
Diazepam or Lorazepam:is used in status epilepticus (fast acting)
Side effects:Very drowsy, tolerance can develop, impair liver (monitor liver studies)
Reversal agent/antodote: Flumazenil
Valproates: Valproic Acid
Use for all types of seizures
Monitor liver, WBC and platelets, GI issues
Medication not working: placement of a vagus nerve stimulator: an electrical device that sends electrical signals to the vagus nerve
Surgery: to remove an area of the brain that is causing the seizure.Example: focal seizures that arise from temporal lobe (temporal lobectomy)